Cancer
Overexpression of splicing protein in skin repair causes early changes seen in skin cancer

|
Normally, tissue injury triggers a mechanism in cells that tries to repair damaged tissue and restore the skin to a normal, or homeostatic state. Errors in this process can give rise to various problems, such as chronic inflammation, which is a known cause of certain cancers.
“It has been noted that cancer resembles a state of chronic wound healing, in which the wound-healing program is erroneously activated and perpetuated,” says Professor Adrian Krainer of Cold Spring Harbor Laboratory (CSHL). In a paper published today in Nature Structural & Molecular Biology, a team led by Dr. Krainer reports that a protein they show is normally involved in healing wounds and maintaining homeostasis in skin tissue is also, under certain conditions, a promoter of invasive and metastatic skin cancers.
The protein, called SRSF6, is what biologists call a splicing factor: it is one of many proteins involved in an essential cellular process called splicing. In splicing, an RNA “message” copied from a gene is edited so that it includes only the portions needed to instruct the cell how to produce a specific protein. The messages of most genes can be edited in multiple ways, using different splicing factors; thus, a single gene can give rise to multiple proteins, with distinct functions.
The SRSF6 protein, while normally contributing to wound healing in skin tissue, when overproduced can promote abnormal growth of skin cells and cancer, Krainer’s team demonstrated in experiments in mice. Indeed, they determined the spot on a particular RNA message - one that encodes the protein tenascin C - where SRSF6 binds abnormally, giving rise to alternate versions of the tenascin C protein that are seen in invasive and metastatic cancers.
United States CDC announces an HPV vaccine recall

|
The United States Centers for Disease Control and Prevention (CDC) was informed by Merck on Monday that the pharmaceutical company planned to recall one lot of Gardasil [Human Papillomavirus Quadrivalent (types 6, 11, 16, and 18) Vaccine, Recombinant].
The CDC media statement released yesterday states that the recall is because a number of vials may contain glass particles as a result of breakage during the vaccine manufacturing process.
Pain drugs used in prostate gland removal linked to cancer outcome, Mayo Clinic-led study finds

|
The methods used to anesthetize prostate cancer patients and control pain when their prostate glands are surgically removed for adenocarcinoma may affect their long-term cancer outcomes, a study led by Mayo Clinic has found. Opioids, painkillers commonly given during and after surgery, may suppress the immune system’s ability to fight cancer cells. The research suggests that supplementing general anesthesia with a spinal or epidural painkiller before a radical prostatectomy reduces a patient’s need for opioids after surgery, and this finding was associated with a lower risk of cancer recurrence. The findings are published online in the British Journal of Anaesthesia.
MULTIMEDIA ALERT: Video of Dr. Sprung is available for download from the Mayo Clinic News Network.
The immune system’s strength is especially important in cancer surgery because surgical manipulation of a tumor may spread cancer cells. The immune system can be impaired by general anesthesia, the overall stress surgery places on the body and by post-surgical systemic opioid use. The study found better outcomes in radical prostatectomy patients who had general anesthesia supplemented with spinal or epidural delivery of a long-acting opioid such as morphine, than in those who received general anesthesia only.
“We found a significant association between this opioid-sparing technique, reduced progression of the prostate tumor and overall mortality,” says senior author Juraj Sprung, M.D., Ph.D., a Mayo Clinic anesthesiologist.
Generic Breast Cancer Drugs Boost Adherence
|
|
The introduction of cheaper, generic aromatase inhibitors, used to prevent breast cancer recurrence, appears to have improved adherence, a researcher said here.
In an analysis of pharmacy claims data, adherence to hormone therapy varied depending on the copayment required, according to Dawn Hershman, MD, of Columbia University in New York City.
But the lower-priced generics had smaller copayments and adherence was greater than for brand name products, Hershman reported at the annual San Antonio Breast Cancer Symposium here.
The findings suggest that efforts should be directed toward reducing financial constraints on patients, as a matter of public health policy, Hershman argued.
New models of drug-resistant breast cancer point to better treatments

|
Human breast tumors transplanted into mice are excellent models of metastatic cancer and are providing insights into how to attack breast cancers that no longer respond to the drugs used to treat them, according to research from Washington University School of Medicine in St. Louis.
The transplanted tumors maintain the genetic errors that caused the original cancer, even though they are growing in mice. As such, mice carrying human tumors can help identify drivers of tumor growth and serve as excellent test subjects for investigating new drugs. The mice are particularly good models of estrogen receptor-positive tumors (so named because they are fueled by estrogen) that have become resistant to the drugs used to treat them.
Matthew J. Ellis, MD, PhD, said the research, presented Dec. 12 at the San Antonio Breast Cancer Symposium, is a step toward precision medicine, allowing scientists to study tumors from patients whose treatment regimens are well-documented.
The researchers, including scientists from The Genome Institute at Washington University School of Medicine, presented the research titled, “Patient-derived xenograft study reveals endocrine therapy resistance of ER+ breast cancer caused by distinct ESR1 gene aberrations.”
Targeted treatment can significantly reduce relapse in children with AML leukemia

|
The addition of a monoclonal antibody called gemtuzumab combined with standard chemotherapy has been shown to significantly reduce the risk of relapse and increase rates of disease-free survival in pediatric patients with acute myeloid leukemia (AML). Post-treatment relapse rates are a major indicator of potential for long-term survival in children with the disease.
The study (abstract #355) evaluated a total of 1,022 children averaging 10 years old at trial sites nationwide, led by Alan Gamis, MD, MPH, Associate Division Director, Section of Oncology at Children’s Mercy Hospital in Kansas City. It will be highlighted in an oral presentation Monday, Dec. 9, at the American Society of Hematology annual meeting in New Orleans.
“Chemotherapy has limits. Particularly in children, increasing doses further can become too toxic for the patient while still not achieving the desired effect on the cancer,” said Dr. Gamis. “This study is significant because it shows for the first time that this targeted treatment can augment the effects of chemotherapy in children and effectively reduce their risk of relapse. We found it was most effective in the patients most at risk.”
Gemtuzumab was removed from the U.S. market in 2010 because the U.S. Food and Drug Administration determined the potential risks of the drug outweighed the potential benefits. Recent research with the compound has raised questions about whether that action may have been premature. This data supports recent findings in adults with AML that gemtuzumab reduced their risk of relapse when added to standard chemotherapy.
Breast tomosynthesis increases cancer detection and reduces recall rates
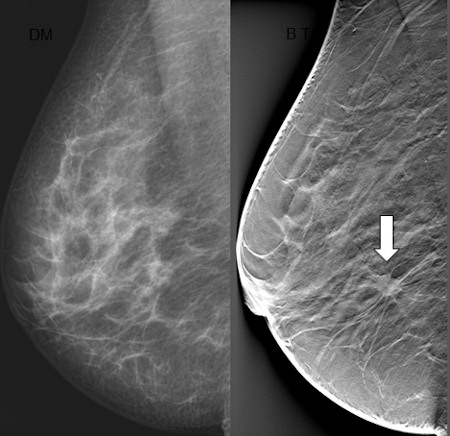
|
Researchers have found that digital breast tomosynthesis (DBT) led to reduced recall rates and an increase in cancer detection in a large breast cancer screening program. The results of this study were presented today at the annual meeting of the Radiological Society of North America (RSNA).
Digital mammography is the gold standard for breast cancer screening, but may yield suspicious findings that turn out not to be cancer. These false-positive findings are associated with a higher recall rate, or the rate at which women are called back for additional imaging or biopsy.
Digital breast tomosynthesis has shown promise at reducing recall rates in all groups of patients, including younger women and women with dense breast tissue. Tomosynthesis is similar to mammography in that it relies on ionizing radiation to generate images of the breast. However, unlike conventional mammography, tomosynthesis allows for three-dimensional (3-D) reconstruction of the breast tissue, which can then be viewed as sequential slices through the breast.
Because DBT technology is relatively new, it is typically used only as a supplemental screening tool, but since October 2011, every patient screened for breast cancer at Hospital of the University of Pennsylvania (HUP) in Philadelphia has been screened using DBT, according to Emily F. Conant, M.D., chief of breast imaging at HUP and the study’s lead author.
Common genetic pathway could be conduit to pediatric tumor treatment
|
|
Investigators at Johns Hopkins have found a known genetic pathway to be active in many difficult-to-treat pediatric brain tumors called low-grade gliomas, potentially offering a new target for the treatment of these cancers.
In laboratory studies, researchers found that the pathway, called mammalian target of rapamycin (mTOR), was highly active in pediatric low-grade gliomas, and that mTOR activity could be blocked using an experimental drug, leading to decreased growth of these tumors.
“We think mTOR could function as an Achilles heel,” says study co-author Eric Raabe, M.D., Ph.D., an assistant professor of pediatrics, oncology and pathology at the Johns Hopkins Kimmel Cancer Center. “It drives cancer growth, but when mTOR is inhibited, the tumor falls apart.” The work was described Nov. 7 in the journal Neuro-Oncology.
Overall, brain tumors affect more than 4,000 children each year in the U.S., and they are the leading cause of cancer deaths in children, according to Raabe. Low-grade gliomas are the most common group of tumors of the central nervous system in children. Current treatments for these tumors include surgery and chemotherapy, which often cause significant side effects. Many of these tumors are located in areas like the optic pathway, where they can’t be easily removed by surgery without causing damage, including blindness. In addition to vision loss, some of Raabe’s patients have endured paralysis or learning problems as a result of the tumor or treatment. “Even though these tumors are considered ‘low grade’ and not particularly aggressive, many patients suffer severe, life-altering symptoms, so we desperately need better therapies,” says Raabe.
Stealth nanoparticles lower drug-resistant tumors’ defenses
|
|
Some of the most dangerous cancers are those that can outmaneuver the very drugs designed to defeat them, but researchers are now reporting a new Trojan-horse approach. In a preliminary study in the journal ACS Nano focusing on a type of breast cancer that is highly resistant to current therapies, they describe a way to sneak small particles into tumor cells, lower their defenses and attack them with drugs, potentially making the therapy much more effective.
Paula T. Hammond and colleagues at the Koch Institute of Integrative Cancer Research at MIT note that triple-negative breast cancer (TNBC) is an aggressive disease that is difficult to treat with standard-of-care therapy, and patients’ prognoses are poor. These cancer cells evade treatment by ramping up the production of certain proteins that protect tumors from chemotherapy drugs. Interfering with this process could give anticancer drugs a better chance at killing resistant tumors. Recent research into molecules called small interfering RNAs, or siRNAs, is opening doors into possible new treatments using this approach. These molecules can halt the production of particular proteins, so they are ideal candidates for dialing down the levels of protective proteins in tumors. But there are challenges to using siRNAs as part of a cancer therapy, so Hammond’s team set out to address them with novel molecular engineering approaches.
They designed a two-stage, “stealth” drug delivery system to attack TNBC cells in mice, often used as stand-ins for humans in research. They created “layer-by-layer” nanoparticles through assembly of components in a certain order around a nano-sized core.
New idea for targeting the common cancer protein KRAS
|
|
Patients with cancers driven by the protein KRAS, which are particularly hard to treat, may benefit from small molecules that attach to and disrupt the function of a KRAS-containing protein complex, according to results presented here at the AACR-NCI-EORTC International Conference on Molecular Targets and Cancer Therapeutics, held Oct. 19-23.
Mutant forms of the protein KRAS are found in approximately 30 percent of all cancers. They are responsible for many of the hallmarks of these cancers, and KRAS is, therefore, considered an important therapeutic target. However, attempts to develop clinically useful KRAS-targeted drugs have been unsuccessful.
“KRAS is a molecular switch,” said Michael Burns, a doctor of medicine and doctor of philosophy candidate at Vanderbilt School of Medicine in Nashville, Tenn. “In the ‘on’ state it transmits signals that drive cell growth and survival. In many cancers, KRAS is permanently in the on state, and it is a highly validated therapeutic target.
“KRAS switches from off to on most efficiently when it is attached to a protein called SOS,” explained Burns. “Each SOS protein attaches to two KRAS proteins, and we have identified a number of small molecules that bind to a particular part of SOS when it is in a complex with two KRAS proteins. These small molecules disrupt the function of the complex, ultimately causing inhibition of the signaling pathways downstream of KRAS that drive cell growth and survival. Although our data were generated in biochemical assays and cell lines, they suggest a potential way to therapeutically target KRAS, which has not been possible to date.”
Pet pig Nemo’s lymphoma treatment makes research history
|
|
When George Goldner went to feed his six pet pigs earlier this year, his 730-pound (331-kg) companion Nemo was acting strangely. Nemo had suddenly stopped eating and laid in the mud.
So Goldner loaded Nemo into a trailer and drove more than two hours to Cornell University Hospital for Animals (CUHA) in Ithaca, New York. There he learned his four-year-old Hampshire pig had what doctors believed was the blood cancer B-cell lymphoma.
The hospital’s researchers told Goldner they had never seen a pig treated for cancer. But that did not deter Goldner, a self-described animal lover, who asked doctors to devise a way to treat his pig based on their knowledge of cancer in dogs and humans and not worry about costs.
2 views are better than 1 in 3-D breast screening
|
|
One view 3D breast screening (tomosynthesis) means less radiation dose and about five seconds less compression, but a study from Yale University, New Haven, CT, found that obtaining both views is necessary to help ensure that a cancer won’t be missed.
There are practices in Europe that have reported performing only a single view, specifically the mediolateral oblique (MLO) view, said Dr. Noa Beck, the lead author of the study. Two views are standard in the U.S. for 3D breast screening; “we wanted to see if one view would be sufficient,” she said. Seven breast imagers reviewed 164 cancers visualized with tomosynthesis and noted on what views the cancers could be seen. The study found that 56% of cancers were equally well seen on both the MLO view and the craniocaudal (CC) view; 34% of the cancers were either better or only seen on the CC view, said Dr. Beck. “The CC view achieves better compression, and this likely explains the reason the CC view showed lesions more clearly. In a few cases, lesions were only seen on the MLO view because of where the cancers were located in the breast,” she said.
The study results emphasize that “obtaining both views is necessary to ensure that a cancer will be optimally visualized,” said Dr. Beck.
Moffitt Cancer Center Researchers Find Potential New Therapeutic Target for Treating Non-Small Cell Lung Cancer
|
|
Researchers at Moffitt Cancer Center have found a potential targeted therapy for patients with tobacco-associated non-small cell lung cancer. It is based on the newly identified oncogene IKBKE, which helps regulate immune response.
The study appeared in the Feb. 13 online issue of Oncogene.
The IKBKE gene is part of a family of enzyme complexes involved in increasing cellular inflammation. IKBKE overexpression has been associated with breast and prostate cancers. However, it had not been linked to environmental carcinogen, such as tobacco smoke, until now.
Tobacco smoke is the strongest documented initiator and promoter of lung cancer. The traditional model holds that tobacco components promote carcinogenesis through a process that leads to DNA damage.
African-Americans still more likely to die from cancer
|
|
Drops in smoking may have helped drive cancer death rates down among black men during the last decade, but they are still more likely to die of cancer than whites, according to a new analysis.
“I think we see some really good news, but then we also see some trends that are going in the wrong direction,” said Carol DeSantis, the study’s lead author from the American Cancer Society (ACS) in Atlanta.
Using information from several databases, the researchers analyzed information on the number of cancers diagnosed and the number of cancer deaths reported across the U.S. between 1990 and 2009.
The biennial analysis found that improvements in cancer treatments and care have avoided nearly 200,000 cancer deaths in blacks since 1990.
Fluid from Pap test used to detect ovarian, endometrial cancers
|
|
Using cervical fluid collected from routine Pap smears, U.S. researchers were able to spot genetic changes caused by both ovarian and endometrial cancers, offering promise for a new kind of screening test for these deadly cancers.
Experts say that although the test has tremendous potential, it is still years from widespread use. But if proven effective with more testing, it would fill a significant void.
Currently, there are no tests that can reliably detect either ovarian or endometrial cancer, which affects the uterine lining. Research teams have been trying for several years to find a screening test that could identify these cancers early, when there is a better chance of a cure.





