Eye / Vision Problems
Joslin researchers find drugs are effective for diabetic macular edema in new trial
|
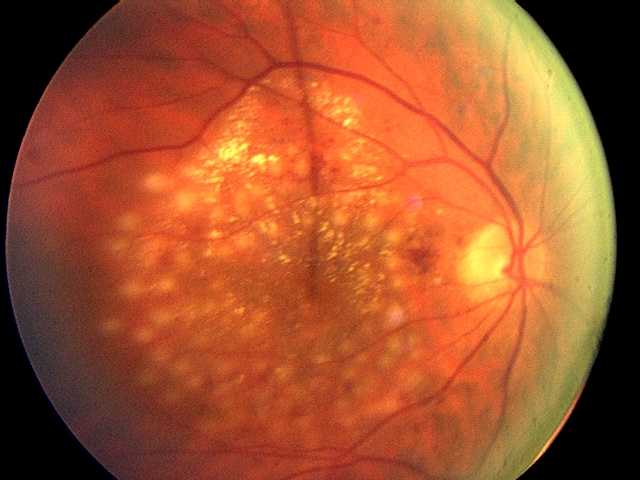
In the first clinical trial directly comparing three drugs most commonly used to treat diabetic macular edema, researchers found all were effective in improving vision and preventing vision loss. However, one drug, aflibercept, provided greater improvement for people with more severe vision loss when treatment was initiated. The trial was conducted by the National Eye Institute Diabetic Retinopathy Clinical Research Network (DRCR.net) including researchers from Joslin Diabetes Center. The results appeared in the February online edition of the New England Journal of Medicine.
Diabetes is a significant risk factor for developing eye diseases. The most common diabetic eye disease and a leading cause of blindness is diabetic retinopathy, which is caused by elevated blood sugar levels damaging the blood vessels of the retina and affects approximately 7.7 million Americans. About 750,000 Americans with diabetic retinopathy have diabetic macular edema (DME) in which fluid leaks into the macula, the area of the retina used when looking straight ahead. The fluid causes the macula to swell, blurring vision. “DME is the leading cause of moderate vision loss in working-age adults with diabetes. With the rate of diabetes increasing dramatically worldwide, many individuals will be at risk for vision loss from diabetic eye complications and DME is a major global health concern,” says Jennifer K. Sun, M.D., M.P.H., a member of the study research team and writing committee, and an Investigator in the Section on Vascular Biology, an ophthalmologist in Beetham Eye Institute at Joslin and an Assistant Professor at Harvard Medical School.
In an earlier study, Joslin researchers reported that VEGF, a major growth factor for blood vessels, is elevated in the eye fluids of patients with proliferative diabetic retinopathy and DME, causing leakage and the growth of abnormal blood vessels.
In the blink of an eye

|
Imagine seeing a dozen pictures flash by in a fraction of a second. You might think it would be impossible to identify any images you see for such a short time. However, a team of neuroscientists from MIT has found that the human brain can process entire images that the eye sees for as little as 13 milliseconds - the first evidence of such rapid processing speed.
That speed is far faster than the 100 milliseconds suggested by previous studies. In the new study, which appears in the journal Attention, Perception, and Psychophysics, researchers asked subjects to look for a particular type of image, such as “picnic” or “smiling couple,” as they viewed a series of six or 12 images, each presented for between 13 and 80 milliseconds.
“The fact that you can do that at these high speeds indicates to us that what vision does is find concepts. That’s what the brain is doing all day long - trying to understand what we’re looking at,” says Mary Potter, an MIT professor of brain and cognitive sciences and senior author of the study.
This rapid-fire processing may help direct the eyes, which shift their gaze three times per second, to their next target, Potter says. “The job of the eyes is not only to get the information into the brain, but to allow the brain to think about it rapidly enough to know what you should look at next. So in general we’re calibrating our eyes so they move around just as often as possible consistent with understanding what we’re seeing,” she says.
UBC-VCH scientists use drug to repair rare birth defect

|
University of British Columbia and Vancouver Coastal Health scientists have developed a potential cure for a rare eye disease, showing for the first time that a drug can repair a birth defect.
They formulated the drug Ataluren into eye drops, and found that it consistently restored normal vision in mice who had aniridia (ANN-uh-ridee- uh), a condition that severely limits the vision of about 5,000 people in North America. A small clinical trial with children and teens is expected to begin next year in Vancouver, the U.S. and the U.K.
Aniridia is caused by the presence of a “nonsense mutation” - an extra “stop sign” on the gene that interrupts production of a protein crucial for eye development. Aniridia patients don’t have an iris (the coloured ring around the pupil), and suffer many other eye abnormalities.
Ataluren is believed to have the power to override the extra stop sign, thus allowing the protein to be made. The UBC-VCH scientists initially thought the drug would work only in utero – giving it to a pregnant mother to prevent aniridia from ever arising in her fetus. But then they gave their specially formulated Ataluren eye drops, which they call START, to two-week-old mice with aniridia, and found that it actually reversed the damage they had been born with.
Higher case load lowers cost of repairing bones that protect eye

|
Adding to evidence that “high-volume” specialty care in busy teaching hospitals leads to efficiencies unavailable in community hospitals, a new study by Johns Hopkins researchers finds that patients undergoing repair of traumatic eye socket injuries at its busy academic medical center fared just as well at far less cost than those treated at all other Maryland hospitals.
The study’s findings, the researchers say, suggest that major cost savings can be had from economies of scale such as utilization of supplies, spending less time in the operating room and potentially from more streamlined pre- and post-operative processes when patients seek eye trauma care at a hospital that specializes in those procedures.
“The presumption has always been that treatment at teaching hospitals is inherently more expensive given the specialized care they provide and the costs of their graduate medical education responsibilities. However, somewhat counter-intuitively, our research shows it’s actually significantly less expensive and just as effective to treat these types of injuries at academic medical centers,” says Michael P. Grant, M.D., Ph.D., director of the Eye and Orbital Trauma Center at the Wilmer Eye Institute at Johns Hopkins. “The cost of health care is on everyone’s minds. Maybe a good way to save money and stretch our health care dollars would be to direct even more patients to the specialists who frequently treat these injuries.”
Grant led the study published in the December issue of the journal Ophthalmology.
Report shows risk of blindness halved over last decade
|
|
Age-related macular degeneration (AMD) is the most frequent cause of blindness in the Western World. A report from the University of Copenhagen and Glostrup Hospital in Denmark published today shows the number of new cases of blindness and severe visual loss in Denmark has been halved during the last ten years.
The study just published in American Journal of Ophthalmology examined the records of 11,848 new cases of legal blindness. The rate of blindness from AMD fell from 522 cases per million inhabitants aged 50 years or older in 2000, to 257 cases per million in 2010, a reduction by over 50 per cent.
The bulk of the decrease occurred after 2006, following the introduction of new effective treatment for wet AMD, which is characterised by leaking blood vessels having formed under the fovea. The treatment consists of repeated injections into the eye of a medication that inhibits the signalling molecule vascular endothelial growth factor (VEGF).
Clustering gene expression changes reveals pathways toward glaucoma prevention
|
|
Glaucoma is the second-most common cause of blindness in the US, and occurs due to loss of retinal ganglion cells and degeneration of the optic nerve. Although it is known that high levels of pressure within the eye predispose individuals to the development of glaucoma, the molecular mechanisms involved are poorly defined.
In new research from The Jackson Laboratory in Bar Harbor, Maine, Simon John and colleagues analyzed gene expression patterns in the retina and optic nerves of mice that develop age-related glaucoma. Using a method that involved the clustering of samples that showed similarity in expression profiles, the researchers were able to identify molecular signatures of early events in glaucoma progression- events that were detectable before there was morphological evidence of damage.
Activation of part of the innate immune system called the complement cascade, and upregulation of endothelin 2- a protein that can increase blood pressure- were among these early changes. Notably, the researchers found that genetically and pharmacologically interfering with these changes protected mice from developing glaucoma.
Sinai Hospital’s Krieger Eye Institute Opens New Retina Center
|
|
The Krieger Eye Institute at Sinai Hospital opened a new center for the treatment of retinal diseases in November. The retina is the layer of tissue at the back of the eye that converts images to electrical impulses. These electrical signals are then perceived by the brain as sight.
The Retina Center treats all retinal diseases including macular degeneration, hypertensive retinopathy, pediatric retinopathy, diabetic retinopathy and sickle cell retinopathy.
“The approach to treating retinal disease has changed drastically in the last few years,” says Donald Abrams, M.D., chief of the Department of Ophthalmology at Sinai Hospital. “This new center allows us to more effectively treat patients suffering from these diseases.”
Eye disorder common among diabetic adults
|
|
Nearly 30 percent of U.S. diabetics over the age of 40 may have a diabetes-related eye disorder, with 4 percent of this population affected severely enough that their vision is threatened, suggests a new study.
The condition, known as diabetic retinopathy, involves damage to the eye’s retina and is the leading cause of new cases of legal blindness among U.S. adults between 20 and 74 years old. It also costs the U.S. approximately $500 million every year.
“The number of people with diabetes is increasing in this country,” lead researcher Dr. Xinzhi Zhang, of the Centers for Disease Control and Prevention in Atlanta, told Reuters Health.
Omega-3s help stave off age-related vision loss
|
|
Want to keep your eyesight sharp as you age? Eating lots of fish packed with healthy omega-3 fatty acids could help, new research suggests.
Among 1,837 people who had early signs of age-related macular degeneration (AMD), those with the highest consumption of omega-3 fatty acids were 30 percent less likely to progress to the advanced form of the disease over a 12-year period than those with the lowest omega-3 intake, researchers found.
Dr. John Paul SanGiovanni of the National Eye Institute at the National Institutes of Health in Bethesda, Maryland, and his colleagues report their findings in the December issue of the American Journal of Clinical Nutrition.
High-dose vitamin C may boost women’s cataract risk
|
|
Women who take high-dose vitamin C supplements may be increasing their risk of age-related cataracts, hint findings of a Swedish study.
Among nearly 24,600 adult women followed for more than 8 years, those who reported regular or occasional vitamin C supplementation of about 1000 milligrams per serving were about 25 percent more likely than those who did not take supplements to have age-related cataracts removed.
Women who took extra vitamin C for 10 years or longer; or in combination with being 65 years and older, or taking hormone replacement or corticosteroid medications had even greater risk, researchers found.
Glaucoma patients overrate their eyedrop skills
|
|
Although more than 90 percent of patients taking ocular medication reported feeling confident about their eyedrop instillation technique, less than one third actually demonstrated adequate skills, researchers report in the Archives of Ophthalmology.
“A large component of adherence to a medical regimen,” investigator Dr. Alan L. Robin told Reuters Health, “is the ability to adequately execute the proper ingestion or instillation of a medication. Physicians often do not dwell on this aspect as they think that one does not have to educate a patient on how to take a pill. However, the proper instillation of an eye drop into the eye is far different than taking a pill.”
Robin went on to point out that apart from it being essential to get a drop into the eye, it’s also important to avoid release of multiple drops, which leads to waste, increased costs and possible inadequate dosing should the medication run out prematurely.
Natural Compound Stops Diabetic Retinopathy
|
|
Oklahoma City, OK—Researchers at the University of Oklahoma Health Sciences Center have found a way to use a natural compound to stop one of the leading causes of blindness in the United States. The research appears online this month in the journal Diabetes, a publication of the American Diabetes Association.
The discovery of the compound’s function in inflammation and blood vessel formation related to eye disease means scientists can now develop new therapies –including eye drops – to stop diabetic retinopathy, a disease which affects as many as five million Americans with Type 1 and Type 2 diabetes.
“There is no good treatment for retinopathy, which is why we are so excited about this work. This opens an entirely new area for pharmaceutical companies to target,” said Jay Ma, the principal investigator on the project and a research partner at the OU Health Sciences Center, Dean A. McGee Eye Institute and the Harold Hamm Oklahoma Diabetes Center.
Retinopathy of prematurity diagnosis time significantly reduced using telemedicine
|
|
To be properly diagnosed, retinopathy of prematurity (ROP), the leading cause of childhood blindness in the United States and worldwide, requires a time intensive process and significant coordination between ophthalmologist and NICU staff. A recent study examining ROP diagnosis speed using indirect ophthalmoscopy versus telemedicine, remote medical consultation, is featured in the July issue of the American Journal of Ophthalmology (http://www.ajo.com), published by Elsevier.
The study was designed to compare the ophthalmologist’s speed of ROP diagnosis using telemedicine versus traditional bedside ophthalmoscopy. The findings reveal that: 1) ROP diagnosis by the ophthalmologist is significantly faster via telemedicine, and 2) there are significant time requirements by ophthalmologists associated with ROP diagnosis at the NICU bedside beyond ophthalmoscopy. In particular, additional time is taken for travel and communication with families and hospital staff.
To counteract these time requirements the implementation of telemedicine for ROP management has the ability to decrease the time commitment for examining ophthalmologists. Previous studies have shown that telemedical ROP diagnosis is highly accurate and reliable compared with ophthalmoscopy, and future work is required to address workflow questions in more detail.
Program offers free eye care to America’s elderly
|
|
Between June 1 and August 31, EyeCare America, a non-profit public service program of the Foundation of the American Academy of Ophthalmology, is offering no-cost medical eye care to qualified seniors.
By the age of 65, one in three Americans has some form of vision-impairing eye disease. The downturn in the U.S. economy has many seniors on fixed incomes struggling with health care costs, including eye care.
Last Updated: 2009-06-11 15:04:35 -0400 (Reuters Health)
Certain foods may thwart age-related vision loss
|
|
A new study suggests that older adults who eat diets rich in citrus fruits, leafy greens and fish oil, but low in “glycemic index,” may have a lower risk of age-related macular degeneration—the leading cause of vision loss among older U.S. adults.
AMD, also known as “age-related macular degeneration” refers to gradual damage to the macula, a structure in the retina that allows for seeing fine detail. The condition affects more than 1 million Americans, usually after the age of 65.
A number of studies have suggested that individual nutrients, including the antioxidants lutein, vitamin C and vitamin E, can help protect against AMD. This latest study, published in the journal Ophthalmology, looked at the overall diet patterns of 4,000 older adults and the links to AMD risk.





