Trauma
Dislocating a hip after total hip replacement can be a traumatic experience

|
Osteoarthritis of the hip is a degenerative joint disease that, besides being painful, also has a negative impact on mobility. An affected joint can be surgically replaced with an artificial prosthesis to alleviate pain and enhance mobility and quality of life. However, when the replacement hip is forced from its normal position-a so-called dislocation-these patients frequently experience injuries, undermining their trust in the artificial joint. Depending on the trauma that caused the dislocation, it may even be necessary to replace the prosthesis. In their current review article published in Deutsches Ärzteblatt International (Dtsch Arztebl Int 2014; 111: 884-90), Jens Dargel et al. point out that the prevention of dislocation plays an important role and describe the risks that need to be addressed.
Approximately 1 in 50 patients who undergo total hip replacement for the first time will experience a dislocation. Among patients with total hip replacements that required revision and implant exchange surgeries, this rate can be as high as 1 in 4 patients (up to 28%). Here the risks include advanced age and concomitant neurological conditions.
Study suggests increase in falls among the elderly

|
Over a 12-year period, the prevalence of self-reported falls among older adults appeared to be on the rise, according to a new nationally representative study.
Falling is the most frequent cause of injury among older adults and about a third of older adults fall each year. Researchers analyzed data from 1998-2010 among adults age 65 and over and found an 8 percent increase in falls - which translates to a relative increase of nearly 30 percent.
The findings appear in JAMA Internal Medicine.
“We expected an increase because older adults are getting older and there are more 80 and 90 year old adults than before, but we were very surprised to find that the increase in falls was not due to the changing demography,” says lead author Christine Cigolle, M.D., M.P.H., assistant professor in the departments of Family Medicine and Internal Medicine at the University of Michigan and a research scientist at the VA Ann Arbor Healthcare System Geriatric Research, Education and Clinical Center (GRECC).
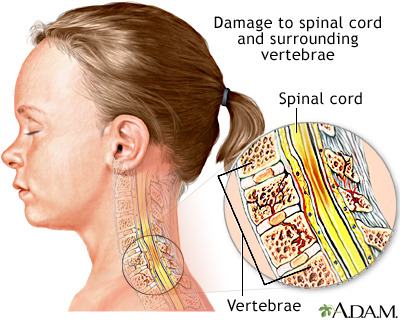
Study finds axon regeneration after Schwann cell graft to injured spinal cord
|
A study carried out at the University of Miami Miller School of Medicine for “The Miami Project to Cure Paralysis” has found that transplanting self-donated Schwann cells (SCs, the principal ensheathing cells of the nervous system) that are elongated so as to bridge scar tissue in the injured spinal cord, aids hind limb functional recovery in rats modeled with spinal cord injury.
The study will be published in a future issue of Cell Transplantation but is currently freely available on-line as an unedited early e-pub at: http://www.ingentaconnect.com/content/cog/ct/pre-prints/content-ct1074Williams.
“Injury to the spinal cord results in scar and cavity formation at the lesion site,” explains study corresponding author Dr. Mary Bartlett Bunge of the University of Miami Miller School of Medicine. “Although numerous cell transplantation strategies have been developed to nullify the lesion environment, scar tissue - in basil lamina sheets - wall off the lesion to prevent further injury and, also, at the interface, scar tissue impedes axon regeneration into and out of the grafts, limiting functional recovery.”
The researchers determined that the properties of a spinal cord/Schwann cell bridge interface enable regenerated and elongated brainstem axons to cross the bridge and potentially lead to an improvement in hind limb movement of rats with spinal cord injury.
Optimal site for cell transplantation to treat spinal cord injury investigated

|
It is known that transplanting neural stem/progenitor cells (NS/PCs) into the spinal cord promotes functional recovery after spinal cord injury (SCI). However, which transplantation sites provide optimal benefit? This question was investigated by a Japanese research team and their findings will be published in a future issue of Cell Transplantation, but are currently freely available on-line as an unedited early e-pub at http://url.health.am/1326/.
“It is critical to determine the optimal transplantation site for NS/PCs aimed at treating SCI,” said Dr. Masaya Nakamura of the Department of Orthopedic Surgery at the Keio University School of Medicine.
Previous work by the same research team revealed that NS/PCs injected into non-injury sites such as by intravenous or intrathecal administration did not engraft to the injury site in sufficient numbers, but instead were often “trapped” in the lungs and kidneys. They concluded that intralesional application might be the most effective and reliable method for transplanting NS/PCs. This study, also using laboratory mice with SCI, sought to determine how effective intralesional injection might be. NS/PCs were obtained from mice transgenic for Venus and luciferase fusion protein, which allowed the cells to be tracked by bioluminescence imaging (BLI) after transplantation.
“Wild-type mice were given a contusive spinal cord injury at the T10 level,” explained Dr. Nakamura. “Low and high doses of NS/PCs derived from fetal transgenic mice were injected into four groups of mice at either the lesion epicenter (E) or at rostral and caudal sites (RC) with neural stem/progenitor cells derived from fetal transgenic mice while a fifth group of controls was injected with phosphate buffered saline at E.”
Degenerative cervical spine disease may not progress over time
|
|
Follow-up data on patients with degenerative disease of the upper (cervical) spinal vertebrae show little or no evidence of worsening degeneration over time, according to a study in the February 15 issue of Spine. The journal is published by Lippincott Williams & Wilkins, a part of Wolters Kluwer Health.
For many patients with “unstable” cervical degenerative spondylolisthesis, observation may be a better choice than surgery, according to the new research by Dr Moon Soo Park and colleagues of Medical College of Hallym University, Republic of Korea. They write, “Our results suggest that the majority of these patients may be stable and do not develop progression of disease or catastrophic neurologic deficits.”
Is Unstable Spondylolisthesis Really Unstable?
The researchers analyzed the “natural history” of cervical degenerative spondylolisthesis in 27 patients. Degenerative spondylolisthesis refers to “slipped” vertebrae caused by bone degeneration. Because spondylolisthesis is commonly thought to result in instability of the cervical spine, spinal fusion surgery (arthrodesis) is sometimes considered the appropriate treatment.
Japan tsunami stress may have brought on seizures: study
|
|
The number of seizure patients in a northern Japanese fishing community devastated by the March 11, 2011 tsunami spiked in the weeks following the disaster, according to a Japanese study.
The study, published in the journal Epilepsia, looked at 440 patient records from Kesennuma City Hospital, in a city that was devastated by the massive tsunami touched off by the 9.0 magnitude earthquake.
Thirteen patients were admitted with seizures in the eight weeks after the disaster, but only one had been admitted in the two months before March 11.
Previous research has linked stressful life-threatening disasters with an increased risk of seizures, but most case reports lacked clinical data with multiple patients.
Development of prosthetic hands stagnated for twenty years
|
|
The development of body-powered prosthetic hands has stagnated for over twenty years. That is the main conclusion of a study by researchers from TU Delft and the University of Groningen into this type of prosthesis, which is published in the American Journal of Rehabilitation Research and Development.
High operating force
The study, which was carried out by researchers from TU Delft and the University of Groningen, measured the force required to operate a number of contemporary body-powered prosthetic hands. The researchers compared the results to earlier measurements from 1987 and came up with remarkable results: today’s prosthetic hands perform equally or less well than those from 1987. The grip strength of the hands is insufficient and a very high operating force is required. Another remarkable result: a prosthetic hand developed in 1945 performed better in the test than the newer prosthetic hands.
Stryker to take charge to end US knee-device probe
|
|
Orthopedic implant maker Stryker Corp said it will take a charge of $33 million in the second quarter for an expected settlement of a U.S. Department of Justice investigation into one of its artificial knee devices.
The charge, which is Stryker’s estimate of what it will cost to settle the probe into marketing practices concerning its OtisKnee device, is expected to reduce its reported diluted earnings per share by about 9 cents in the second quarter, Stryker said. The Kalamazoo, Michigan-based company said it will exclude the charge from its adjusted earnings per share.
In 2010, Stryker received a subpoena alleging violations of laws prohibiting sales of a medical device not cleared for marketing by the U.S. Food and Drug Administration.
High-level trauma care may limit disability
|
|
People treated for severe injuries at a specialized trauma center may survive with fewer disabilities than those at other hospitals, a study from Australia suggests.
The findings, researchers say, add to evidence that patients fare better when they’re treated under an organized trauma system - where hospitals, emergency services and state governments have coordinated plans for getting the right patients to the appropriate treatment.
So-called Level I trauma centers provide the most comprehensive care for traumatic injuries and have to meet certain requirements - like having a specific number of surgeons and other specialists on duty 24 hours a day.
Risk of Blood Loss in Childhood Back Surgery Varies with Cause of Spine Deformity
|
|
The relative risk of blood loss during corrective spine surgery in children appears linked to the underlying condition causing the spinal deformity, according to a new study from Johns Hopkins Children’s Center.
Results of the study, published online March 15 in the journal Spine, can help surgeons prepare, plan and safeguard against this common and serious complication, the investigators say. Blood loss during surgery can increase the length of hospital stay, lead to complications and portend worse overall outcomes.
The Johns Hopkins investigation, believed to be the first to explore the link between intraoperative blood loss and pediatric patients’ underlying condition, is based on an analysis of 617 cases of children, ages 10 through 18, who had surgery to fuse bones to stabilize and correct a spine deformity. All surgeries were conducted at Johns Hopkins between 2001 and 2011.
Researchers Find Epidural Steroid Injections Do Not Benefit Spine Patients
|
|
Researchers at the Rothman Institute at Jefferson examined data on patients being treated for lumbar stenosis and the degenerative spine condition spondylolisthesis and found that patients who received epidural steroid injections (ESI) had a higher rate of crossover to surgery and fared worse in physical health and bodily pain versus those who did not receive ESI, dispelling their pre-study hypothesis.
Data for this study was gathered from the database of the prospective, multicenter NIH-funded SPORT (Spine Patient Outcomes Research Trial) of surgical treatment versus nonoperative treatment for lumbar stenosis and degenerative spondylolisthesis. In the first three months of the trial, some patients were given ESI and some were not.
“At the onset of our study, we hypothesized that patients who received ESI would have improved outcomes and lower rates of surgery compared to patients who did not receive ESI,” said Kristen E. Radcliff, MD, of the Rothman Institute at Jefferson and an author on the study. “This was not supported by the data.”
College Athlete Died of Head Trauma, Father Says
|
|
A 22-year-old football player for Frostburg State University in Maryland has died from head trauma sustained on the field, his father said.
Nearly a week after passing out during a routine practice, fullback Derek Sheely died late Sunday at the University of Maryland R Adams Cowley Shock Trauma Center in Baltimore.
Kenneth Sheely, Derek’s father, said in a telephone interview from the family’s home in Germantown, Md., that he was told by doctors that Derek had sustained “severe head trauma.”
Injured patients fare slightly better on weekends
|
|
Injured patients who are treated by trauma teams at hospitals are less likely to die when they are admitted on weekends versus weekdays, new research from Pennsylvania shows.
The results contrast with studies of intensive care units and stroke patients that have revealed a “weekend effect,” in which patients landing in the hospital from Friday night to Monday morning are more likely to have complications or die (see Reuters Health reports, July 6, 2010 and November 1, 2010).
The researchers looked at records from Pennsylvania hospitals, including more than 90,000 patients over a 5-year period. All the patients came in with an injury, for instance from a gunshot or car accident.
Helicopter Transport Increases Survival for Seriously Injured Patients
|
|
Severely injured patients transported by helicopter from the scene of an accident are more likely to survive than patients brought to trauma centers by ground ambulance, according to a new study published in The Journal of Trauma: Injury, Infection, and Critical Care. The study is the first to examine the role of helicopter transport on a national level and includes the largest number of helicopter-transport patients in a single analysis.
The finding that helicopter transport positively impacts patient survival comes amid an ongoing debate surrounding the role of helicopter transport in civilian trauma care in the United States, with advocates citing the benefits of fast transport times and critics pointing to safety, utilization and cost concerns.
The new national data shows that patients selected for helicopter transport to trauma centers are more severely injured, come from greater distances and require more hospital resources, including admission to the intensive care unit, the use of a ventilator to assist breathing and urgent surgery, compared to patients transported by ground ambulance. Despite this, helicopter-transport patients are more likely than ground-transport patients to survive and be sent home following treatment.
Biomarker Identified for Predicting Increased Risk of Developing Post Traumatic Epilepsy
|
|
Approximately 5 – 30% of patients with traumatic brain injury (TBI) develop post traumatic epilepsy (PTE). The onset of seizures in patients who are susceptible to PTE can range from weeks or months to more than a decade after TBI. In a presentation today at the 64th American Epilepsy Society annual meeting, scientists report that the analysis of routine MRI scans can reliably quantify the disruptions in the blood brain barrier that are increasingly believed to be a prominent contributor to epilepsy development.
Investigators at the University of Colorado used MRI imaging to differentiate brain injured and sham injured laboratory animals. At three months post-injury, the animals were administered a substance known to provoke seizures. The investigators found that the degree of blood brain barrier disruption (BBBD) observed in the images was significantly correlated with the total number of seizures occurring in the first 60 minutes after the substance was administered, as well as correlating with how soon after drug administration the seizures began. (Platform A.05)
According to Dr. Lauren Frey, lead author of the report, “The significant correlation we found between the images and post-injury seizure susceptibility supports the presence of blood brain barrier disruption as a biomarker for posttraumatic epileptogenesis.”





