Weight Loss
Don’t Blame Breast Density; $$$ Toxicity; ‘Nurse Ratched’ Returns
|
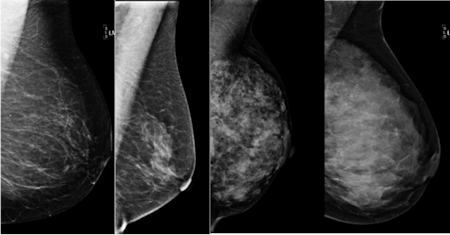
Age and body weight, not breast-tissue density, drive a woman’s risk of breast cancer, according to a study from Johns Hopkins.
An 8-year-old Utah girl has developed only the 35th known case of secretory breast carcinoma, a rare form of breast cancer that occurs in young girls.
The “financial toxicity” of cancer is not unique to the U.S., as an American oncologist learned over dinner with two colleagues practicing in the nation of Georgia.
Two pediatric oncologists share their insights into to dealing with the “unsung heartache” of caring for children with cancer.
Early Heart Data Look Good for Obesity Drug

|
Interim data from a cardiovascular safety study of an investigational weight-loss agent have met FDA criteria, and drugmaker Orexigen Therapeutics will seek to resubmit the drug for U.S. approval.
A company press release reported that the combination of naltrexone and bupropion (Contrave) didn’t double the risk of major adverse cardiovascular events (MACE) compared with placebo - a requirement set by the FDA - in an interim look at data from the Light Study, a cardiovascular outcomes trial.
The drug was denied FDA approval in February 2011, even though an advisory committee had voted largely in favor of approval. The agency required that the company conduct a cardiovascular outcome trial before it would approve the drug.
It also agreed that if the study could exclude a doubling of the risk of MACE with the drug compared with placebo, the company could submit the interim analysis for consideration in a resubmitted new drug application (NDA).
Sexual function dramatically improves in women following bariatric surgery, Penn study finds
|
|
The first study to look extensively at sexual function in women who underwent bariatric surgery found that significant improvements in overall sexual function, most reproductive hormones and in psychological status were maintained over two years following surgery. Women reporting the poorest quality of sexual function prior to surgery saw the most dramatic improvements one year after surgery, on par with women who reported the highest quality of sexual function prior to surgery. The new report by researchers with the Perelman School of Medicine at the University of Pennsylvania appears in the November 4 edition of JAMA Surgery.
More than half of women who seek bariatric surgery report signs of sexual dysfunction and, consequentially, psychological stress.
“For many people, sex is an important part of quality of life. The massive weight losses typically seen following bariatric surgery are associated with significant improvements in quality of life,” said the study’s lead author David Sarwer, PhD, professor of Psychology in Psychiatry and Surgery in the Perelman School of Medicine at the University of Pennsylvania. “This is one of the first studies to show that women also experience improvements in their sexual functioning and satisfaction, as well as significant improvements in their reproductive hormones.”
Researchers followed 106 women with an average Body Mass Index of 44.5 who underwent bariatric surgery (85 had gastric bypass and 21 had gastric banding procedures). Following surgery, the women lost an average of 32.7 percent of their original body weight after the first year, and 33.5 percent at the end of the second year.
Glowing fish shed light on metabolism
|
|
A tiny, translucent zebrafish that glows green when its liver makes glucose has helped an international team of researchers identify a compound that regulates whole-body metabolism and appears to protect obese mice from signs of metabolic disorders.
Led by scientists at the University of California, San Francisco (UCSF), the work demonstrates how a fish smaller than a grain of rice can help screen for drugs to help control obesity, type 2 diabetes and other metabolic disorders, which affect a rising 34 percent of American adults and are major risk factors for cardiovascular disease.
Described this week in the journal Nature Chemical Biology, the new compound emerged from a panel of 2,400 medications and drug-like compounds tested in the zebrafish. The test was designed to identify key regulators of “fasting metabolism”- a state most people face every day after the lingering remnants of their long-digested meals pass slowly down their digestive tract.
Fasting metabolism is the body’s way of fulfilling its energy needs between meals by turning to fat and other stored sources. It involves a carefully balanced and coordinated cascade of reactions that see numerous genes in various tissues kick into action and do things like burn fat.
Gastric bypass for weight loss increases alcohol use, study says
|
|
A major new study confirms previous sporadic reports that weight-loss surgery increases the risk of alcohol abuse, researchers reported Monday. In the second year after having a gastric bypass, technically known as Roux-en-Y surgery, patients were 30% more likely to have problems controlling their alcohol use, a team reported online in the Journal of the American Medical Assn. and at the annual meeting of the American Society for Metabolic and Bariatric Surgery.
Previous reports have suggested that alcohol abuse could be a problem following bariatric surgery, but the studies have been small and generally involved collecting data at some point after the procedure. In the new study, a team led by epidemiologist Wendy C. King of the University of Pittsburgh School of Medicine began studying 2,458 adults before they underwent bariatric surgery at one of 10 hospitals. Of those, 1,945 could be monitored for one to two years after the procedure.
The team found that 7.6% of the patients suffered from alcohol-abuse disorders (abuse and dependence) in the year before the surgery. At the end of one year after the procedure, the percentage was about the same, 7.3%. But by the end of the second year, the prevalence of such disorders had climbed to 9.6%, a 30% increase. Virtually all of the increase occurred in patients who had undergone gastric bypass, with no increase among the roughly 30% of patients who had a banding procedure.
Obesity Costs Twice as Much
|
|
As politicians and pundits debate the repeal of President Obama’s health care plan, a new study shows that the treatment of obesity could fall under greater scrutiny when the legislation takes effect. The reason? Medical costs related to obesity may be twice as high as earlier estimates, according to one new report.
The study analyzed the actual weight of people, while previous studies only considered the self reported weight of patients, which was likely to be understated. Researchers also took into account the role of genetic factors in the patients, looking at the weight of each subject’s immediate family members to determine whether obesity ran in the family.
Researchers John Cawley, Ph.D., an associate professor at Cornell University, and Chad Meyerhoefer, Ph.D., professor of economics at Lehigh University, based their findings on data from a survey involving 24,000 adult patients from 2000 to 2005. They found that costs related to obesity medical care are close to $168 billion, representing 17 percent of medical costs in the U.S. The figure is a sizeable jump from last year’s estimate of $147 billion – a figure cited by federal health officials – which is 9 percent of the country’s total medical costs.
Patients with diabetes may need fewer medications after bariatric surgery
|
|
Bariatric surgery appears to be associated with reduced use of medications and lower health care costs among patients with type 2 diabetes, according to a report in the August issue of Archives of Surgery, one of the JAMA/Archives journals.
“The rapidly growing epidemics of obesity and diabetes threaten to overburden the world’s health care systems,” the authors write as background information in the article. “From an epidemiological standpoint, once these diseases develop they are rarely reversed. Dietary, pharmaceutical and behavior treatments for obesity are associated with high failure rates, and medical management of diabetes is also often unsuccessful. Despite many efforts to improve the control of glucose levels in diabetes, including clinical guidelines and patient and provider education, less than half of all patients with type 2 diabetes mellitus achieve the American Diabetes Association recommendation of a hemoglobin A1C level of less than 7 percent.”
The use of bariatric surgery—that results in long-term weight loss, improved lifestyle and decreased risk of death—has tripled in the past five years, the authors note. Martin A. Makary, M.D., M.P.H., and colleagues at the Johns Hopkins Bloomberg School of Public Health and The Johns Hopkins University School of Medicine, Baltimore, studied 2,235 U.S. adults (average age 48.4) with type 2 diabetes who underwent bariatric surgery during a four-year period, from 2002 to 2005. They used claims data to measure the use of diabetes medications before and after surgery, along with health care costs per year.
Sleep problems linked to weight gain in middle-age
|
|
Women, try not to think of this if you lie awake at night: having trouble sleeping means you’re likely to gain weight.
As if simply getting older weren’t hard enough, new research shows that middle-aged and older women who have trouble falling or staying asleep may pack on more pounds than their well-rested contemporaries.
A number of studies have found that sleep-deprived children and adults are more likely to be overweight than those who usually get a full night’s rest. But many of those studies assessed people at one point in time, so it was hard to know which came first, the sleep problems or the excess pounds.
Community interventions and in-home visits may slow excess weight gain in American Indian children
|
|
Community intervention can help American Indian families change behavior related to early childhood weight gain and obesity, according to a new Kaiser Permanente and Northwest Portland Area Indian Health Board (NPAIHB) study.
The study, published online in the Journal of Community Health, also finds that adding in-home visits to the community intervention has an even more profound effect on behavior change, and can reduce a child’s body mass index.
Funded by the National Institutes of Health, this is the first study to target obesity prevention among American Indian children starting at birth.
Eating Breakfast Boosts Weight Loss
|
|
If you’re skipping breakfast in an effort to slim down, it might be wise to rethink your weight-loss strategy. Studies show that folks who eat breakfast tend to be thinner and healthier than those who don’t.
In a study of nearly 3,000 individuals enrolled in the National Weight Control Registry (NWCR), 78 percent reported eating breakfast every day of the week. All NWCR subjects had maintained a weight loss of 30 pounds for at least one year. On average, the subjects had lost more than 70 pounds and kept it off for six years.
Skipping any meal — especially breakfast — seems to promote weight gain rather than weight loss, since breakfast-skippers are more likely to give in to mid-morning munchies or extra-large lunches. Either way, they typically end up consuming far more calories than if they had just eaten breakfast in the first place.
Obesity May be Evaded by Weight Loss Surgery
|
|
Complication arising in pregnancy due to obesity can be evaded with weight loss surgery. If overweight women undergo weight loss surgery before they conceive, it may avert pregnancy complications.
It is known that women who are overweight have a high chance of developing complexities during pregnancy. One example of such complication is high blood pressure, or preeclampsia, which elevates the threat of premature birth and infant death.
Wendy L. Bennett, M. D., M. P. H., Assistant Professor of Medicine at the Johns Hopkins University School of Medicine and lead researcher evinces, “We have long known that women who have these blood pressure disorders are not only at an increased risk for pregnancy complications in themselves and their babies, but also for chronic diseases in the future” .
Vitamin D, Weight Loss, and Obesity
|
|
Vitamin D continues to make headline news. Findings suggest adequate levels may break barriers with individuals battling excess weight.
Research reveals a relationship between vitamin D levels in the body, vitamin D intake, and body weight. While the exact relationship is not entirely understood, a growing body of evidence suggests an association between obesity/excess body weight and D levels exists.
In addition, the link is supported by the fact that obesity and low D are co morbid (occur at the same time) with diseases such as: disease, hypertension, diabetes, osteoarthritis, osteoporosis, depression and even periodontal disease.
Lap-Band Weight-Loss Surgery Can Reverse Metabolic Syndrome in Obese Teens
|
|
A new study of obese adolescents has shown that laparoscopic gastric banding surgery—the “Lap-Band” procedure—not only helps them achieve significant weight loss but can also improve and even reverse metabolic syndrome, reducing their risk for cardiovascular disease and diabetes.
Metabolic syndrome is defined as a cluster of risk factors—high blood pressure; low levels of HDL or “good” cholesterol; excessive abdominal fat; and elevated levels of blood sugar, C-reactive protein and triglycerides—that increase a person’s chances of developing cardiovascular disease or diabetes later in life. The single biggest risk factor is obesity, and metabolic syndrome usually improves when a person loses weight.
The study was led by Drs. Ilene Fennoy, Jeffrey Zitsman and colleagues at NewYork-Presbyterian Morgan Stanley Children’s Hospital and Columbia University Medical Center and presented at the annual Endocrine Society meeting in Washington, D.C.
Gastric bypass provides long-term diabetes control
|
|
In more than half of obese patients with type 2 diabetes, their metabolic condition resolves after gastric bypass and they remain free from diabetes up to 16 years later, according to study findings presented last week at the 26th Annual Meeting of the American Society for Metabolic and Bariatric Surgery in Dallas.
In a study of 177 patients with diabetes who underwent gastric bypass for obesity, also referred to as bariatric surgery, between 1993 and 2003, the severity of diabetes before surgery was a key predictor of whether diabetes resolved in the long term. Moreover, long-term diabetes resolution correlated with the maintenance of weight loss.
“The most significant finding is that long-term resolution of diabetes seems to be linked to how severe the diabetes was at the time of surgery,” senior author Dr. James W. Maher, from Virginia Commonwealth University, Richmond, told Reuters Health. “Patients with diet-controlled diabetes had a 75 percent likelihood of being diabetes-free at long-term followup, while the figure was 65 percent diabetes-free in patients who were originally controlled with oral medications and only 28 percent of insulin-dependent diabetics had long-term resolution.”
Hormone May Help Combat Frailty in Older Women
|
|
Frail elderly women with unexplained weight loss may benefit from supplementation with the body’s appetite-stimulating hormone, ghrelin, or with similar agents, according to a new study. Results of the study, which was funded partially by the National Institutes of Health, were presented at The Endocrine Society’s 91st Annual Meeting in Washington, D.C.
Unexplained weight loss is a common problem in older adults. It can lead to the development of frailty, a debilitating syndrome of declines across multiple body systems.
Frail individuals have much higher rates of functional decline, hospitalization and death than healthier people their age, said study lead investigator Anne Cappola, MD, ScM, assistant professor of medicine at the University of Pennsylvania School of Medicine, Philadelphia.





