HPV vaccination not associated with increase in sexually transmitted infections

|
A barrier to human papillomavirus (HPV) vaccination has been the concern that it may promote unsafe sexual activity, but a new study of adolescent girls finds that HPV vaccination was not associated with increases in sexually transmitted infections (STIs), according to an article published online by JAMA Internal Medicine.
Nearly one-quarter of U.S. females between the ages 14 and 19 and 45 percent of women between the ages of 20 and 24 are affected by HPV. The HPV vaccination can prevent cervical, vulvar and vaginal cancers and genital warts caused by certain HPV strains. Still, HPV vaccination rates remain low in the United States and, by 2013, only 57 percent of females between the ages of 13 and 17 had received at least one dose, whereas only 38 percent had received all three recommended doses, according to the study background.
Anupam B. Jena, M.D., Ph.D., of Harvard Medical School, Boston, and coauthors used a large insurance database of females (ages 12 to 18) from 2005 through 2010 to examine STIs among girls who were vaccinated and those who were not.
Study identifies 8 signs associated with impending death in cancer patients

|
Researchers at The University of Texas MD Anderson Cancer Center have identified eight highly specific physical and cognitive signs associated with imminent death in cancer patients. The findings, published in the journal Cancer, could offer clinicians the ability to better communicate with patients and families. They may also guide both the medical team and caregivers on complex decision making, such as discontinuation of tests and therapy, plans for hospital discharge and hospice referral.
Previous studies in end-of-life care have focused on physicians prognosticating better. However, according to David Hui, M.D., assistant professor, Palliative Care and Rehabilitation Medicine, research on how to tell if a patient has entered the final days of life has been minimal. Knowing with a high degree of confidence that death is imminent could have significant implications for clinical practice. It may also help families and caregivers make more informed decisions.
“In the past, studies trying to understand the signs associated with impending death were conducted in people who were recognized as dying, so there’s a potential bias built into this model. With our study, we observed a list of signs in patients from the time they were admitted to the palliative care unit. They were observed systematically, twice a day, without knowing if the patient would die or be discharged,” says Hui, the study’s corresponding author.
BGI study confirms accuracy of its NIFTY in nearly 147,000 pregnancies

|
BGI has published a study tracking the clinical performance of its whole genome sequencing-based non-invasive prenatal test (the NIFTY® test) in nearly 147,000 pregnancies, the largest such study to date. The results showed high sensitivity and specificity and no significant difference between high-risk and low-risk pregnant women.
The study, published in the journal Ultrasound Obstetrics and Gynecology, reported on 146,958 samples from 508 medical centers in mainland China, which were collected between early 2012 and mid-2013 for trisomy 21, 18, and 13. Although NIFTY® measures other chromosomal abnormalities, these results were not included in the study.
According to the study’s results, NIFTY® identified 1,578 trisomy-positive and 145,380 negative samples. Comparing the results with follow-up confirmatory invasive testing, or by tracking patients’ eventual pregnancy outcomes, the study team then calculated the false positive (FPR) and false negative rate (FNR) for each tested trisomy, and the overall sensitivity, specificity, and positive predictive value (PPV).
Hepatitis C more prevalent than HIV/AIDS or Ebola yet lacks equal attention

|
More than 180 million people in the world have hepatitis C, compared with the 34 million with HIV/AIDS and the roughly 30,000 who have had Ebola. Yet very little is heard about the hepatitis C virus (HCV) in the way of awareness campaigns, research funding or celebrity fundraisers.
One of the global regions highly affected by hepatitis C is West Africa. In developed countries, hepatitis C, a blood-borne disease, is transmitted through intravenous (IV) drug use. “In West Africa, we believe that there are many transmission modes and they are not through IV drug use, but through cultural and every day practices,” says Jennifer Layden, MD, PhD principal investigator on a study recently published in the journal Clinical Infectious Diseases. “In this study, tribal scarring, home birthing and traditional as opposed to hospital based circumcision procedures, were associated with hepatitis C infection in Ghana.”
The study was conducted by HepNet, an international multidisciplinary group of physicians and scientists. “The other important finding was that a high percentage of individuals who tested positive for HCV had evidence of active infection,” says Layden. “This illustrates the need for treatment.”
Discovering the source of the disease and a target population, she says, will aid in the next step of the research: how to protect and prevent the disease in Ghana.
Physician guidelines for Googling patients need revisions

|
With the Internet and social media becoming woven into the modern medical practice, Penn State College of Medicine researchers contend that professional medical societies must update or amend their Internet guidelines to address when it is ethical to “Google” a patient. “As time goes on, Googling patients is going to become more and more common, especially with doctors who grew up with the Internet,” says Maria J. Baker, associate professor of medicine. Baker has dealt with the question first hand in her role as a genetic counselor and medical geneticist. In a case that inspired her recent paper in the Journal of General Internal Medicine, a patient consulted her regarding prophylactic mastectomies. The patient’s family history of cancer could not be verified and then a pathology report revealed that a melanoma the patient listed had actually been a non-cancerous, shape-changing mole.
Turning to the Internet, Baker found evidence of the patient capitalizing on being a cancer victim for a cancer she did not have. The question, Baker says, is in what circumstances is it appropriate for a doctor to research a patient using online search engines? “Googling a patient can undermine the trust between a patient and his or her provider, but in some cases it might be ethically justified,” Baker says. “Healthcare providers need guidance on when they should do it and how they should deal with what they learn.”
With regard to future guidelines, Baker and her co-authors suggest 10 situations that may justify patient-targeted Googling:
How negative stereotyping affects older people

|
The most comprehensive analysis to date of research on the effect of negative stereotypes on older people’s abilities has concluded that these stereotypes create a significant problem for that demographic.
A research team at the University of Kent’s School of Psychology carried out a review and meta-analysis of Aged-Based Stereotype Threat (ABST).
They statistically analysed international evidence from 37 research studies, both published and unpublished. They concluded that older adults’ memory and cognitive performance is negatively affected in situations that signal or remind them of negative age stereotypes. These effects affect both men and women.
The research, funded by the Economic and Social Research council (ESRC), was carried out by Ruth Lamont, working with Dr Hannah Swift and Professor Dominic Abrams. It further found that older people’s cognitive performance suffers more when the threat is induced by stereotypes rather than by facts.
Researchers identify efficient methylating enzyme for cancer development
|
A recent study may help begin to explain how cancer develops though the abnormal turning on and off of genes. Researchers have discovered that the increase of methyl tags in cancer cells is due to highly efficient DNA methyl transferase 1 (DNMT1) enzymes found in these cells. The findings appear in the Journal of Proteomics and Bioinformatics.
Both plants and animals have genetic machinery that modifies the information and function of their genomes without actually changing their genetic code. This modification process is known as “epigenetics.” One of the best studied of these epigenetic processes involves the chemical tagging of DNA nucleotides across the genome using methyl groups. These “methyl tags” are attached to cytosine nucleotides in specific patterns around genes and other expressed sequences by a specialized group of enzymes called methyltransferases.
Genes that are expressed and turned into proteins are free of “methyl” tags, but when such methyl tags attach to DNA, gene expression is turned off. “Whether methyl tags are added to genes varies during normal development and during the development of diseases like cancer, and understanding these processes is currently a major topic of research,” explained corresponding author Sibaji Sarkar, PhD, instructor of medicine at Boston University School of Medicine (BUSM). According to Sarkar it was previously discovered that cancer cells have more methyl tags than normal cells and level of the enzyme which adds the tag, DNA methyl transferase1 (DNMT1) is also higher, but no one knew that both increases are not proportional.
Gene may open door for improved keloid, scar treatment
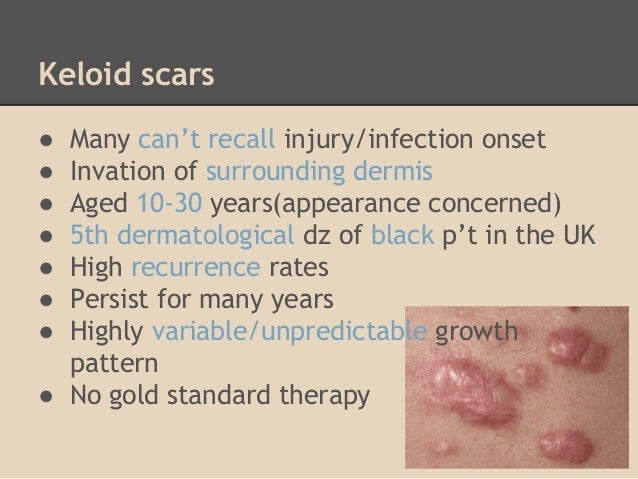
|
Researchers at Henry Ford Hospital in Detroit have identified a gene that may offer a better understanding of how keloid scars develop and potentially open the door to improved treatment for the often painful, itchy and tender scars.
The study is the first to demonstrate that an altered AHNAK gene may have a significant biological role in keloid development.
“This finding has great promise for better understanding how keloids function and offer a potential target for improved and novel treatments,” says study lead author Lamont R. Jones, M.D., Vice Chair, Department of Otolaryngology-Head and Neck Surgery at Henry Ford.
“We now have a better understanding of how this gene fits in the broader picture of the wound healing process, which may be important in preventing scars in general.”
Dislocating a hip after total hip replacement can be a traumatic experience

|
Osteoarthritis of the hip is a degenerative joint disease that, besides being painful, also has a negative impact on mobility. An affected joint can be surgically replaced with an artificial prosthesis to alleviate pain and enhance mobility and quality of life. However, when the replacement hip is forced from its normal position-a so-called dislocation-these patients frequently experience injuries, undermining their trust in the artificial joint. Depending on the trauma that caused the dislocation, it may even be necessary to replace the prosthesis. In their current review article published in Deutsches Ärzteblatt International (Dtsch Arztebl Int 2014; 111: 884-90), Jens Dargel et al. point out that the prevention of dislocation plays an important role and describe the risks that need to be addressed.
Approximately 1 in 50 patients who undergo total hip replacement for the first time will experience a dislocation. Among patients with total hip replacements that required revision and implant exchange surgeries, this rate can be as high as 1 in 4 patients (up to 28%). Here the risks include advanced age and concomitant neurological conditions.
SPECTAcolor viable next generation multinational cancer clinical trial infrastructure

|
SPECTAcolor’s successful start has demonstrated its viability to facilitate next generation cancer clinical trials. It has been successfully implemented across 19 clinical centers located in nine countries in Europe, has now recruited over 500 patients since its launch in September 2013, and the observed frequency of mutations is similar to that observed in previous colorectal cancer clinical trials. In addition, pathological review and core analyses of tumor blocks shipped to the central biobank at Dresden University Hospital for central quality deemed over 98% of the samples were adequate. This successful implementation is evidence that a logistically complex infrastructure to run next generation trials in a multinational setting is feasible.
These results were presented by SPECTAcolor coordinator Dr. Gunnar Folprecht of the Dresden University Hospital at the 2015 Gastrointestinal Cancers Symposium held 15-17 January 2015 in San Francisco.
J Clin Oncol 33, 2015 (suppl 3; abstr 575)
Treatments for patients with cancer are becoming more and more tailored to the molecular characteristics of the particular patient and disease. Consequently, molecularly characterizing a patient’s disease is now a prerequisite for them to access the appropriate clinical trial for their particular cancer. Assessing their tumor, however, is more easily said than done, because the required testing is beyond the scope of most hospitals. Cancer is too diverse, so the EORTC built a collaborative molecular screening platform, SPECTAcolor, which provides the necessary infrastructure to screen adult patients with advanced stage colorectal cancer for mutations in colorectal cancer biomarkers.
Study suggests increase in falls among the elderly

|
Over a 12-year period, the prevalence of self-reported falls among older adults appeared to be on the rise, according to a new nationally representative study.
Falling is the most frequent cause of injury among older adults and about a third of older adults fall each year. Researchers analyzed data from 1998-2010 among adults age 65 and over and found an 8 percent increase in falls - which translates to a relative increase of nearly 30 percent.
The findings appear in JAMA Internal Medicine.
“We expected an increase because older adults are getting older and there are more 80 and 90 year old adults than before, but we were very surprised to find that the increase in falls was not due to the changing demography,” says lead author Christine Cigolle, M.D., M.P.H., assistant professor in the departments of Family Medicine and Internal Medicine at the University of Michigan and a research scientist at the VA Ann Arbor Healthcare System Geriatric Research, Education and Clinical Center (GRECC).
Cell-associated HIV mucosal transmission: The neglected pathway

|
Dr. Deborah Anderson from Boston University School of Medicine (BUSM) and her colleagues are challenging dogma about the transmission of the human immunodeficiency virus type 1 (HIV-1). Most research has focused on infection by free viral particles, while this group proposes that HIV is also transmitted by infected cells. While inside cells, HIV is protected from antibodies and other antiviral factors, and cell-to-cell virus transmission occurs very efficiently through intercellular synapses. The Journal of Infectious Diseases (JID) has devoted their December supplement to this important and understudied topic.
The 10 articles, four from researchers at BUSM, present the case for cell-associated HIV transmission as an important element contributing to the HIV epidemic. Anderson chides fellow researchers for not using cell-associated HIV in their transmission models: “The failure of several recent vaccine and microbicide clinical trials to prevent HIV transmission may be due in part to this oversight.”
Approximately 75 million people in the world have been infected with HIV-1 since the epidemic started over 30 years ago, mostly through sexual contact and maternal-to-child transmission. A series of vaccine and microbicide clinical trials to prevent HIV transmission have been unsuccessful, and scientists are returning to the drawing board to devise new approaches. The JID supplement advocates for new strategies that target HIV-infected cells in mucosal secretions.
New technique provides novel approach to diagnosing ciliopathies
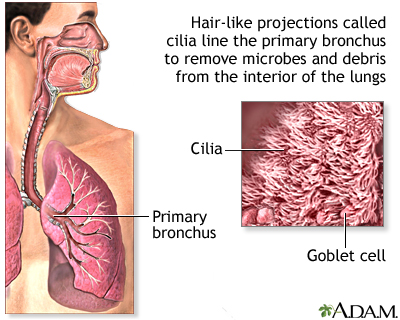
|
Cilia, the cell’s tails and antennas, are among the most important biological structures. They line our windpipe and sweep away all the junk we inhale; they help us see, smell and reproduce. When a mutation disrupts the function or structure of cilia, the effects on the human body are devastating and sometimes lethal.
The challenge in diagnosing, studying and treating these genetic disorders, called ciliopathies, is the small size of cilia—about 500-times thinner than a piece of paper. It’s been difficult to examine them in molecular detail until now.
Professor Daniela Nicastro and postdoctoral fellow Jianfeng Lin have captured the highest-resolution images of human cilia ever, using a new approach developed jointly with Lawrence Ostrowski and Michael Knowles from the University of North Carolina School of Medicine. They reported on the approach in a recent issue of Nature Communications.
About 20 different ciliopathies have been identified so far, including primary ciliary dyskinesia (PCD) and polycystic kidney disease (PKD), two of the most common ciliopathies. They are typically diagnosed through genetic screening and examination of a patient’s cilia under a conventional electron microscope.
UTSW researchers identify a therapeutic strategy that may treat a childhood neurological disorder

|
UT Southwestern Medical Center researchers have identified a possible therapy to treat neurofibromatosis type 1 or NF1, a childhood neurological disease characterized by learning deficits and autism that is caused by inherited mutations in the gene encoding a protein called neurofibromin.
Researchers initially determined that loss of neurofibromin in mice affects the development of the part of the brain called the cerebellum, which is responsible for balance, speech, memory, and learning.
The research team, led by Dr. Luis F. Parada, Chairman of Developmental Biology, next discovered that the anatomical defects in the cerebellum that arise in their mouse model of NF1 could be reversed by treating the animals with a molecule that counteracts the loss of neurofibromin.
“Children with neurofibromatosis have a high incidence of intellectual deficits and autism, syndromes that have been linked to the cerebellum and cortex,” said Dr. Parada, Director of the Kent Waldrep Foundation Center for Basic Neuroscience Research and holder of the Diana K. and Richard C. Strauss Distinguished Chair in Developmental Biology and the Southwestern Ball Distinguished Chair in Nerve Regeneration Research at UT Southwestern. “Our findings in these mouse models suggest that despite embryonic loss of the gene, therapies after birth may be able to reverse some aspects of the disease.”
Advance Directives Can Benefit Patients, Families, and Health Care System

|
Nearly one out of four older Americans say that either they or a family member have experienced excessive or unwanted medical treatment, according to the latest issue of The Gerontological Society of America’s Public Policy & Aging Report (PP&AR), which goes on to show that Americans strongly support holding doctors accountable when they fail to honor patients’ end-of-life health care wishes.
This PP&AR, titled “Advanced Illness Care: Issues and Options,” features 12 articles that present new ways of understanding the complexity of securing appropriate advanced illness care and the decision-making dilemmas it presents. It also provides a valuable benefit by reviewing specific programs, demonstrations, and tools that family members and providers can use in providing care to persons with advanced illness. These models are person- and family-centered, and preliminary evaluations find that they may be cost-effective as well. Support for the publication was provided by Compassion & Choices.
“It is important to ensure that patients and their wishes are what drive the health care system, particularly at the end of life,” said Daniel R. Wilson, the national and federal programs director for Compassion & Choices. “We were pleased to partner with The Gerontological Society of America to publish this issue of the PP&AR, which includes cutting edge writers and thinkers in the advanced illness and end-of-life field.”





