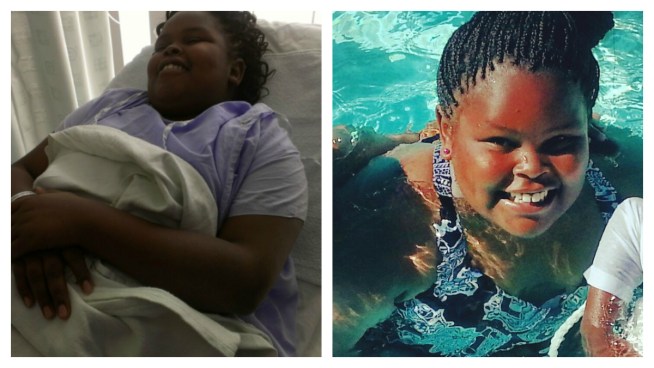
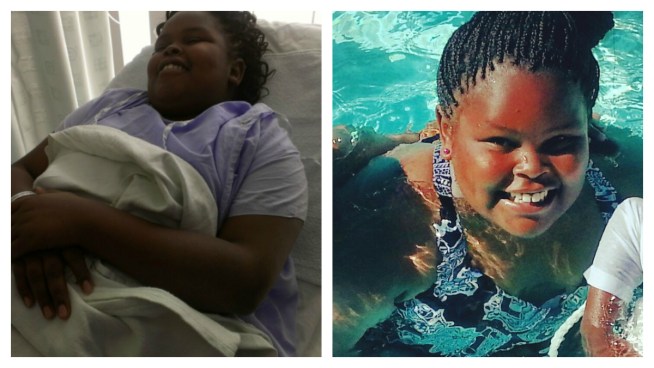
California girl to be kept on life support
|
A 13-year-old California girl declared brain dead after complications from a tonsillectomy should be kept on life support for the time being, a judge has ruled.
The family of Jahi McMath says doctors at Children’s Hospital Oakland wanted to disconnect life support after Jahi was declared brain dead on Dec. 12.
Friday’s ruling by Superior Court Judge Evelio Grillo came as both sides in the case agreed to get together and chose a neurologist to further examine Jahi and determine her condition. The judge scheduled a hearing Monday to appoint a physician.
The girl’s family sought the court order to keep Jahi on a ventilator. They left the courtroom without commenting.
After her daughter underwent a supposedly routine tonsillectomy and was moved to a recovery room, Nailah Winkfield began to fear something was going horribly wrong.
Jahi was sitting up in bed, her hospital gown bloody, and holding a pink cup full of blood.
“Is this normal?” Winkfield repeatedly asked nurses.
 With her family and hospital staff trying to help and comfort her, Jahi kept bleeding profusely for the next few hours then went into cardiac arrest, her mother said.
With her family and hospital staff trying to help and comfort her, Jahi kept bleeding profusely for the next few hours then went into cardiac arrest, her mother said.
Despite the family’s description of the surgery as routine, the hospital said in a memorandum presented to the court Friday that the procedure was a “complicated” one.
“Ms. McMath is dead and cannot be brought back to life,” the hospital said in the memo, adding: “Children’s is under no legal obligation to provide medical or other intervention for a deceased person.”
In an interview at Children’s Hospital Oakland on Thursday night, Winkfield described the nightmarish turn of events after her daughter underwent tonsil removal surgery to help with her sleep apnea.
She said that even before the surgery, her daughter had expressed fears that she wouldn’t wake up after the operation. To everyone’s relief, she appeared alert, was talking and even ate a Popsicle afterward.
But about a half-hour later, shortly after the girl was taken to the intensive care unit, she began bleeding from her mouth and nose despite efforts by hospital staff and her family.
While the bleeding continued, Jahi wrote her mother notes. In one, the girl asked to have her nose wiped because she felt it running. Her mother said she didn’t want to scare her daughter by saying it was blood.
Family members said there were containers of Jahi’s blood in the room, and hospital staff members were providing transfusions to counteract the blood loss.
“I don’t know what a tonsillectomy is supposed to look like after you have it, but that blood was un-normal for anything,” Winkfield said.
The family said hospital officials told them in a meeting Thursday that they want to take the girl off life support quickly.
“I just looked at the doctor to his face and I told him you better not touch her,” Winkfield recalled.
The family filed a request Friday for a temporary restraining order prohibiting the hospital from taking Jahi off life support or any of her other current treatment.
At the hearing later, the hospital’s attorney, Doug Straus, said two doctors unaffiliated with the hospital examined Jahi and concluded that she was brain dead. But he said, “We’re happy to cooperate with the judge’s suggestion that an independent expert be provided to confirm yet again that brain death is the outcome that has occurred here.”
The family’s attorney, Christopher Dolan, said the family wanted independent tests of their own because they do not believe the hospital’s physicians are sufficiently independent.
“There is mistrust and there is a conflict of interest,” he said.
Judge Grillo said he would grant the restraining order in hopes that a resolution could be reached by Christmas to give the family peace of mind.
Hospitals do a barrage of sophisticated tests to determine brain death, said Dr. Cristobal Barrios, an associate professor and a trauma and critical care surgeon at the University of California, Irvine. He is not involved in Jahi’s care and spoke about general hospital protocols.
The tests include touching a patient’s cornea to elicit a blink, moving a breathing tube to stimulate a gag reflex, tickling the back of the throat to bring on a cough, and applying pressure or pain.
If the patient fails to respond to all of those tests, doctors remove the breathing tube for a few minutes. If there is any brain activity, the patient should begin breathing within a few minutes, he said.
In some cases, doctors will also draw a blood sample, add radioactive tags and re-inject it into the body to track where it flows. If the blood doesn’t flow to the brain, Barrios said, there is no brain activity.
Generally, two teams of specialists must run the tests and determine independently that the patient is brain dead, he said. At UC Irvine, those evaluations must take place 12 hours apart if the patient is a child.
Barrios said it’s not unusual for family members to resist a diagnosis of brain death.
While the hospital is not obligated to keep life support going after that diagnosis, Barrios has left brain dead patients hooked up for up to five days while family members move toward acceptance, he said.
“I understand why sometimes for families it’s devastating and confusing,” he said.
—-
Associated Press writer Gillian Flaccus in Santa Ana contributed to this report.
###
By By Terry Collins
Print Version
Tell-a-Friend comments powered by Disqus





