Study finds axon regeneration after Schwann cell graft to injured spinal cord
|
A study carried out at the University of Miami Miller School of Medicine for “The Miami Project to Cure Paralysis” has found that transplanting self-donated Schwann cells (SCs, the principal ensheathing cells of the nervous system) that are elongated so as to bridge scar tissue in the injured spinal cord, aids hind limb functional recovery in rats modeled with spinal cord injury.
The study will be published in a future issue of Cell Transplantation but is currently freely available on-line as an unedited early e-pub at: http://www.ingentaconnect.com/content/cog/ct/pre-prints/content-ct1074Williams.
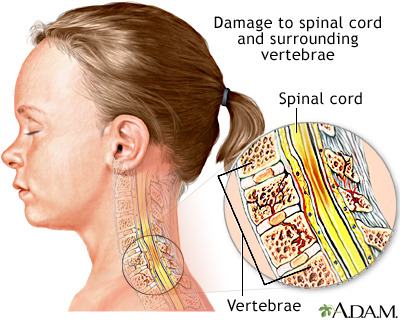
“Injury to the spinal cord results in scar and cavity formation at the lesion site,” explains study corresponding author Dr. Mary Bartlett Bunge of the University of Miami Miller School of Medicine. “Although numerous cell transplantation strategies have been developed to nullify the lesion environment, scar tissue - in basil lamina sheets - wall off the lesion to prevent further injury and, also, at the interface, scar tissue impedes axon regeneration into and out of the grafts, limiting functional recovery.”
The researchers determined that the properties of a spinal cord/Schwann cell bridge interface enable regenerated and elongated brainstem axons to cross the bridge and potentially lead to an improvement in hind limb movement of rats with spinal cord injury.
Electron microscopy revealed that axons, SCs, and astrocytes were enclosed together within tunnels bounded by continuous basal lamina. The expression of neuroglycan (NG2; a proteoglycan found on the membrane of cells) was associated with these tunnels. They subsequently determined that a “trio” of astrocyte processes, SCs and regenerating axons were “bundled” together within the tunnels of basal lamina.
“Elongation of astrocyte processes across transplant interfaces likely establishes three-dimensional structures that determine how regenerating axons become exposed to myriad growth-promoting and inhibitory cues,” wrote the researchers. The researchers also noted that it was important to understand conditions that favor astrocytes to be permissive for axonal growth into lesion transplants.
“We demonstrated that the elongation of astrocyte processes into SC transplants, and the formation of NG2+ tunnels, enables brainstem axon regeneration and improvement in function,” they concluded. “This study supports the clinical use of SCs for SCI repair and defines important characteristics of permissive spinal cord/graft interfaces.”
“Developing the means to bridge the glial scar following chronic spinal cord injury is one of the major stumbling blocks of therapy” said Dr. John Sladek, Cell Transplantation section editor and professor of neurology and pediatrics at the University of Colorado School of Medicine. “This study provides important new insight into how this may be achieved”.
###
Contact: Dr. Mary Bartlett Bunge, The Miami Project to Cure Paralysis, Lois Pope Life Center, PO Box 016960, R-48, Miami, FL 33101, USA
Email: .(JavaScript must be enabled to view this email address)
Tel: 305-243-4596
Fax: 305-243-3923
Citation: Williams, R. R.; Henao, M.; Pearse, D. D.; Bunge, M. B. Permissive Schwann Cell Graft/Spinal Cord Interfaces For Axon Regeneration. Cell Transplant. Appeared or available online: October 22, 2013
The Coeditors-in-chief for CELL TRANSPLANTATION are at the Diabetes Research Institute, University of Miami Miller School of Medicine and Center for Neuropsychiatry, China Medical University Hospital, TaiChung, Taiwan. Contact, Camillo Ricordi, MD at .(JavaScript must be enabled to view this email address) or Shinn-Zong Lin, MD, PhD at .(JavaScript must be enabled to view this email address) or David Eve, PhD at .(JavaScript must be enabled to view this email address)
###
Robert Miranda
.(JavaScript must be enabled to view this email address)
Cell Transplantation Center of Excellence for Aging and Brain Repair
Print Version
Tell-a-Friend comments powered by Disqus





